Download PDF (1.5 MB, 12 pp.) To view a PDF file, you'll need Adobe Acrobat Reader on your comp uter. Acrobat Reader may be downloaded from the Adobe Web site
Text Only Version (below)

Published by the Research and Training Center on Community Living, Institute on Community Integration • College of Education and Human Development, University of Minnesota
Volume 21 • Number 3 • December 2011
A National Review of Home and Community Based Services (HCBS) for Individuals with Autism Spectrum Disorders
This Policy Research Brief summarizes the results of a national study on the status of Home and Community Based Services (HCBS) for persons with autism spectrum disorders (ASD). The purpose of the study was to investigate how people with ASD are being served across states in Home and Community Based Services, including service eligibility, state trends specific to autism services, and lessons learned. The study was conducted at the University of Minnesota’s Research and Training Center on Community Living (RTC), in collaboration with the Minnesota Leadership Education in Neurodevelopmental Disabilities (MN LEND) program at the University. It reports data gathered in 2009-2010. This brief was authored by Jennifer Hall-Lande, Ph.D., Research Project Coordinator at the RTC; Amy Hewitt, Ph.D., Director of the RTC and Training Director of MN LEND; and Charles R. Moseley, Ed.D., Associate Executive Director of the National Association of State Directors of Developmental Disabilities Services. The study was supported by Grant #H133B080005 from the National Institute on Disability and Rehabilitation Research, U.S. Department of Education, to the RTC; and by Grant #T73MC12835 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), to the Department of Pediatrics, University of Minnesota. For further information, please contact Jennifer Hall-Lande at hall0440@umn.edu.
Introduction
Autism spectrum disorders (ASD) are among the fastest-growing developmental disability diagnosis in the United States. It is estimated that approximately 1.5 million individuals in this country have an ASD diagnosis. Most recent estimates from the Centers for Disease Control and Prevention (CDC) indicate that 1 in 110 children are currently diagnosed with an autism spectrum disorder (Centers for Disease Control and Prevention, 2010; Kogan et al., 2009). While the number of children diagnosed with ASD is increasing rapidly, the number of adults with ASD is less clear and less easy to reliably measure. A recent study estimated that approximately 1% of the adult population has an ASD diagnosis (Brugha et al., 2009). Further, research reports estimate that the population of individuals that represent the first wave of what is sometimes called the “autism epidemic” is now entering adulthood (Gerhardt, 2009).
Autism spectrum disorders are complex neurodevelopmental disabilities with significant impairments in important functional skills such as communication and socialization. Diagnosis is based on the presence of an identified set or spectrum of behaviors that can affect individuals in different ways. Common characteristics of people with ASD include restricted, narrow interests and repetitive behaviors. Signs typically appear before age 3 and persist throughout the lifespan. While some individuals with ASD develop typical functional skills, many display a broad range of ongoing intellectual, behavioral, social, and emotional limitations.
Autism spectrum disorders are lifelong conditions that often require expensive supports and intensive interventions (Cavagnaro, 2007; Cimera & Cowan, 2009). Cognitive disabilities are present in an estimated 59% of individuals with autism (Baird et al., 2006; Kim et al., 2011). However, recent research suggests that as clinical knowledge of ASD evolves, more individuals who receive an ASD diagnosis may not have intellectual disabilities as currently defined (Edelson, 2006). Although a specific causal brain mechanism associated with ASD has yet to be found, researchers have found structural brain annomalies in children with ASD (Uddin et al., 2011).
The prevalence of ASD diagnosis has been steadily increasing since the 1990s. State educational data on ASD suggest a 10-17% annual growth in nationwide prevalence (U.S. State Educational Data, 2003; Cavagnaro, 2007). Other sources reflect more significant increases in the educational disability category of ASD. For example, a review of special education services conducted by Larson and Lakin (2010) reported a 349.2% increase in special education ASD diagnosis between 1999 and 2008. To date, there is not a single, universally-accepted explanation for the increase in prevalence. This increase is likely due to various factors, including increased public awareness, changes in diagnostic criteria, improved availability of services and supports, and an emphasis placed on diagnosis occurring at an earlier age. While there is no agreement on a single cause for the increase in diagnosis, the current evidence available does not rule out the possibility that ASD may be becoming more prevalent (Lord & Bishop, 2009).
The increase in ASD diagnoses highlights the need for high quality, accessible services and supports that extend across the lifespan. Historically, such services and supports have been both vital and costly. It is estimated that approximately $35 billion is spent annually on both direct and indirect supports for people with ASD and their families (Ganz, 2007). The available, yet limited, research suggests that the lifetime cost of supporting an individual diagnosed with ASD ranges from $2.5 million to $4.4 million per person (Ganz, 2006, 2007; Jacobson, Mulick, & Green, 1998; Järbrink & Knapp, 2001). Approximately 60% of these expenditures are estimated to be related to adult services. Without modifications to current systems, the significant expense associated with supporting people with ASD is expected to rise in coming years (Gerhardt, 2009).
Research suggests that the cost of lifelong supports may be cut by as much as two-thirds with early diagnosis and appropriate intervention (Järbrink & Knapp, 2001). Some early intervention cost-benefit analyses have estimated the lifetime savings per individual with an ASD (ages 3-55 years) may range from $656,000 to $1,082,000 (Jacobson, Mulick, & Green, 1998). Research also points to significant cost savings if intervention is targeted appropriately and if there is a good support match for individuals and families with ASD. Current ASD-related services may be expensive partly because of a lack of coordination of support services.
Systems and supports are emerging to accommodate the early detection and intervention needs of children with ASD. The research on children with ASD is clear: Intervene early with intensive services and supports therapy (Courchesne & Pierce, 2005; Dawson et al., 2009; Ozonoff & Cathcart, 1998). There appears to be a critical window of early intervention for behavioral therapy during the childhood years of birth through age 5. Further, the American Academy of Pediatrics has released recommendations for ASD screening in children between the ages of 18 to 24 months (Johnson & Myers, 2007).
While a number of new specialized services and supports are emerging to meet the needs of children with ASD, the research literature has devoted less attention to issues concerning adults with ASD (Howlin, Goode, Hutton, & Rutter, 2004; Hurlbutt & Chalmers, 2004). Of the literature that exists, the majority of individuals with ASD appear to have consistently poor adult outcomes (Eaves & Ho, 2008; Mawhood, Howlin, & Rutter, 2000; Saldana et al., 2009). Previous research reports significant challenges for adults with ASD, including persistent problems in communication, social relationships, social interactions, social isolation, and independence. Success in employment among adults with ASD is also a significant problem (Cimera & Cowan, 2009).
A recent study (National Core Indicators, 2008) reveals many interesting trends for adults with ASD served by state developmental disability service systems. Challenges with communication, social skills, and behavior appeared to significantly influence access to independent living and self-determination. Compared to other individuals with intellectual and/or developmental disabilities (ID/DD) in state service systems, people with ASD were, as a group, more likely to live in their family home than in independent or group home settings, and were less likely to experience personal choice and control in major life decisions. While outcomes for adults with ASD have been consistently poor, research has also revealed that one of the most significant indicators of quality of life for individuals with ASD is the quality of supports and services (Renty & Roeyers, 2006).
Staff and support systems are often challenged to meet the needs of many people with ASD. The wide spectrum of issues around communication, social, and behavioral functioning create both complexities and challenges to effective intervention. Research on community living for people with disabilities consistently reports that individuals with disabilities (such as ASD) and their families need person- and family-centered services tailored to individual and family needs and strengths. Supports must also be customized to the unique needs of the individual with ASD with a balance of accessibility and flexibility to meet the changing, diverse needs of the individual and the family (Freedman & Boyer, 2000; Hurth, Shaw, Izeman, Whaley, & Rogers, 1999).
Until the 1980s, adults with ASD who did not live with family members, like those with other intellectual and developmental disabilities, were primarily served in public and private institutions and larger group homes certified as Intermediate Care Facilities for the Mentally Retarded (ICF-MR) and funded as an optional service under states’ Medicaid programs. Changes to Title XIX of the Social Security Act in 1981 included new provisions under section 1915(c) permitting states to request a waiver of the ICF-MR provisions for the purpose of providing home and community based services to eligible individuals who, if not for the waiver, would be served in institutions. In subsequent years, states’ HCBS waiver programs became the primary source of funding support for individuals with intellectual disabilities and related conditions (such as autism, cerebral palsy, and others) and their families. States develop and operate their own HCBS programs based on state needs, priorities, and legislative direction. Nationally, in 2009, section 1915(c) served 562,067 people with intellectual and/or developmental disabilities at a total cost of $24.7 billion (Lakin, Larson, Salmi, & Webster, 2010). In fiscal year 2009, HCBS expenditures were nearly double the amount of ICF-MR spending ($12.6 billion). Approximately 90,348 people with ID/DD are served in ICF-MR programs nationwide. Of this number about one-third of all ICF-MR residents live in state-operated institutions, with the balance residing in privately-operated ICF-MR facility-based programs serving four or more people. ICF-MR services typically include a combination of traditional medical supports (e.g., physician care, dental care, nursing services) and non-medical services (e.g., case management, respite care, community living modifications/supports).
The eligibility process involves two separate determinations. First, a person must meet Medicaid eligibility requirements based on income and other provisions such as the Tax Equity and Fiscal Responsibility Act of 1982. People eligible for Medicaid may qualify for ICF-MR services if they meet the institutional level of care criteria. People are eligible for ICF-MR services, and by extension HCBS services, if they have been determined to have intellectual disabilities or a related condition and, for the ICF-MR program, need “active treatment.” People who meet the state’s eligibility criteria may receive supports in an institution or, preferably, in the community under the state’s 1915(c) waiver program(s). Just as Medicaid eligibility may vary from one state to another, so too may states’ eligibility for HCBS waiver program services and services funded by local state dollars. Some states, for example, use a categorical approach for determining eligibility, limiting services to individuals with certain categories of diagnosis, such as intellectual disability, cerebral palsy, or ASD. Other states use functional skills criteria that are based on an individual’s adaptive skills (i.e., ability to perform activities of daily living at norm-referenced, specified levels). Most states combine these two approaches in their eligibility definition, requiring applicants to meet both functional skill and categorical disability criteria. All states incorporate some type of income guidelines into HCBS eligibility (Zaharia & Moseley, 2008).
There are challenges to the current HCBS waiver being used for long-term services and supports for people with ASD. Historically, these systems were designed to meet the needs of people with intellectual disabilities and are not specifically designed for people with ASD. In some states, people with ASD do not meet categorical eligibility criteria. When the diagnosis of autism and/or ASD is not included in the eligibility definitions, an individual’s qualification of an intellectual disability (i.e., an intelligence quotient below 70-75 and adaptive behavior limitations) is the defining factor. As a result, people with ASD who have borderline, average or above-average cognitive abilities are typically ineligible for services under HCBS waiver programs (U.S. Government Accountability Office, 2006).
Limited access to HCBS is exacerbated by state programs that are typically overburdened with high demand for services and limited funding. The increase in the number of youth and adults with support needs has placed increased challenges on an adult service system that already has longstanding waitlists (Zaharia & Moseley, 2008). States can limit the number of individuals enrolled in their HCBS waiver programs. In many states, waiting lists for enrollment can be several years long. Some states have begun to reshape HCBS to address this new demand.
Specialized funding and support services for youth and adults with ASD have not kept pace with the increasing numbers of persons being identified as having ASD and in need of services. Further, there appears to be a significant shortage of trained professionals and specialized services – including speech/language therapy, occupational therapy, behavioral supports, and supported community living services – to meet the diverse needs of individuals with ASD. This shortage of specialized services and well-trained professionals to support people with ASD creates significant challenges for adults in accessing the full range of services they need to live independently in community settings (U.S. Government Accountability Office, 2006).
This Policy Research Brief provides an overview of state policy related to HCBS waivers and ASD. It also offers a discussion of key differences across states in the inclusion of people with ASD in the HCBS program, the presence of specific autism waivers, and definitions of ASD-based eligibility. A discussion of the policy implications is included at the end of this brief.
Methodology
The study summarized here examined the extent to which states have included people with ASD in their HCBS waiver services and how states serve individuals with ASD under the HCBS Medicaid waiver. Specific questions asked were:
- Does your state have a related clause in your Home and Community Based Services (HCBS) waiver for serving people with autism?
- Does your state have a [specific HCBS] waiver exclusively for people with autism who need home and community based services?
- What criteria or documentation do people with autism need to qualify for services in your state?
The study integrated three data collection activities. First, a thorough review of the Centers for Medicare and Medicaid Services (CMS) Web site was conducted in 2009-2010 to determine: (a) the states that specifically included ASD as a related condition/clause in their primary HCBS waiver application, and (b) the states that had a specific autism waiver. Second, the Web sites of state departments of human services/disabilities were reviewed to learn about the HCBS for people with ASD in specific states. The state criteria for ASD eligibility was also included in the state Web site review. Finally, when the information on HCBS could not be found via the state Web site, a follow-up call or e-mail was made to key staff at the state’s department of developmental disabilities services. These follow-up calls and/or e-mails occurred in 2010.
When policy was unclear on the state and CMS Web sites, attempts were made to follow-up with state departments about existing ASD policy. If state personnel did not respond, multiple attempts were made to obtain accurate results. When there were discrepancies between posted state policy and state staff responses, multiple attempts were made to clarify policy. That said, the collected data is only as reliable as the information provided to the research team. Furthermore, it is important to recognize that with the heightened attention on ASD, state policy is in flux and data gathered in this survey may already be outdated in some states. The findings presented here represent a snapshot in time and reflect policy during the period of data collection.
Findings
Several important findings emerged from this study. They fall under the categories of: (a) waiver status across states, (b) eligibility under HCBS waiver, (c) autism-specific waivers, (d) eligibility for adult autism waivers, and (e) services on autism-specific waivers.
Waiver Status Across States
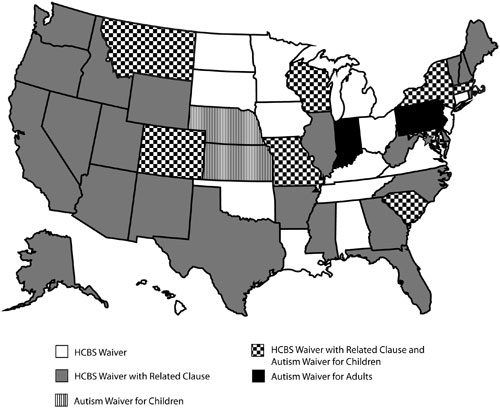
At the time of the interviews, all 50 states and the District of Columbia (D.C.) reported serving people with intellectual disabilities under one or more of their section 1915(c) or section 1115 Medicaid waiver programs. The waivers in most states used broad categories when describing who was targeted for services in their comprehensive HCBS waiver, such as, “serves individuals with Developmental Disabilities, Intellectual Disabilities, Mental Retardation, etc.” Although many states serve people with ASD under their primary HCBS waiver, not all states explicitly included ASD as a specific related-conditions clause. At the time of this data collection, 33 states and the District of Columbia listed autism as a related clause or explicitly included autism in the definition of people served under the state’s HCBS waiver for people with intellectual disabilities. Figure 1 is a map of the United States that reflects the status of the HCBS and autism-specific waivers across the states at the time of the interviews. States with comprehensive HCBS programs that primarily served people with intellectual and/or developmental disabilities and did not have a specific autism clause are shown in white. States shown in gray offered HCBS to persons with intellectual and/or developmental disabilities with explicit inclusion (i.e., related clause) of people with autism. States shown with a line pattern included a children’s autism waiver under their main HCBS MR/DD waiver. States shown with a “checkerboard” pattern had both a HCBS waiver with related clause and an autism waiver for children. States shown in black had a special waiver that served adults with autism. Table 1 summarizes the state waiver information and includes data on the number of individuals served in ICF-MR and HCBS programs for individuals with intellectual and developmental disabilities (Lakin, Larson, Salmi, & Webster, 2010).
| Figure 1: Status of HCBS and Autism-Specific Waivers Across the United States in 2009-2010 | |
|---|---|
|
|
As seen in Table 1, most states, including Alaska, Arizona, Arkansas, California, Colorado, Delaware, D.C., Florida, Georgia, Idaho, Illinois, Indiana, Maine, Maryland, Massachusetts, Mississippi, Missouri, Montana, Nevada, New Hampshire, New Mexico, New York, North Carolina, Oregon, Pennsylvania, Rhode Island, South Carolina, Texas, Utah, Vermont, Washington, West Virginia, Wisconsin, and Wyoming stated that individuals with autism were included in one or more of their HCBS programs for persons with intellectual and/or developmental disabilities (the latter sometimes referred to as “related conditions”). A few, yet growing, number of states reported having autism-specific waivers for children. At the time this data was collected, 11 states offered autism-specific waivers for children. As shown in Table 1, Colorado, Indiana, Kansas, Maryland, Massachusetts, Missouri, Montana, Nebraska, New York (ASD/DD/MR), South Carolina (PDD waiver), and Wisconsin (Children’s DD waiver) had autism waivers specific only to children. Two states, Indiana and Pennsylvania, had autism waivers that specifically served adults.
Table 1: State Waivers and Data on the Number of Individuals Served in the ICF-MR and HCBS Programs in 2009-2010 |
|||||
| State | Autism Related Clause |
Autism Waiver for Children |
Autism Waiver for Adults |
ICF-MR |
Waiver |
| AL | 233 |
5,460 |
|||
| AK | X |
0 |
1,248 |
||
| AZ | X |
200 |
21,811 |
||
| AR | X |
1,598 |
3,744 |
||
| CA | X |
9,293 |
80,862 |
||
| CO | X |
X |
115 |
7,883 |
|
| CT | 1,080 |
8,519 |
|||
| DE | X |
120 |
831 |
||
| DC | X |
443 |
1,338 |
||
| FL | X |
3,100 |
29,807 |
||
| GA | X |
761 |
11,433 |
||
| HI | 91 |
2,586 |
|||
| ID | X |
535 |
2,484 |
||
| IL | X |
8,525 |
15,302 |
||
| IN | X |
X |
X |
4,129 |
10,961 |
| IA | 2,056 |
13,983 |
|||
| KS | X |
521 |
7,749 |
||
| KY | 623 |
5,073 |
|||
| LA | 4,988 |
7,616 |
|||
| ME | X |
183 |
4,212 |
||
| MD | X |
X |
129 |
11,162 |
|
| MA | X |
X |
866 |
11,861 |
|
| MI | 0 |
8,535 |
|||
| MN | 1,747 |
14,832 |
|||
| MS | X |
2,644 |
1,974 |
||
| MO | X |
X |
785 |
8,766 |
|
| MT | X |
X |
52 |
2,273 |
|
| NE | X |
427 |
3,728 |
||
| NV | X |
100 |
1,567 |
||
| NH | X |
25 |
4,108 |
||
| NJ | 2,865 |
10,081 |
|||
| NM | X |
231 |
3,885 |
||
| NY | X |
X |
7,664 |
62,195 |
|
| NC | X |
3,854 |
10,333 |
||
| ND | 584 |
3,805 |
|||
| OH | 6,136 |
24,312 |
|||
| OK | 1,616 |
5,248 |
|||
| OR | X |
22 |
10,884 |
||
| PA | X |
X |
3,939 |
30,393 |
|
| RI | X |
38 |
3,275 |
||
| SC | X |
X |
1,445 |
5,768 |
|
| SD | 146 |
2,901 |
|||
| TN | 1,089 |
7,548 |
|||
| TX | X |
10,792 |
19,795 |
||
| UT | X |
780 |
4,214 |
||
| VT | X |
6 |
2,372 |
||
| VA | 1,606 |
8,662 |
|||
| WA | X |
760 |
10,831 |
||
| WV | X |
477 |
4,334 |
||
| WI | X |
X |
847 |
17,424 |
|
| WY | X |
82 |
2,099 |
||
| ICF-MR and waiver data source: Lakin, Larson, Salmi, & Webster, (2010). | |||||
Eligibility Under HCBS Waiver
Zaharia and Moseley (2008) found that state eligibility definitions fall into three broad categories: intellectual disabilities, intellectual disabilities and related conditions, and developmental disabilities. There are variations on these categorical themes, but states basically used one of the following for eligibility determination:
- The definition of developmental disabilities from the Developmental Disabilities Assistance and Bill of Rights Act of 2000.
- Criteria that require a minimum diagnosis of intellectual disability. Persons with other specified related conditions are eligible as long as they have intellectual disabilities. Related conditions that qualify are specifically identified in the eligibility definitions in many of those states. Some states allow some flexibility for children.
- Eligibility criteria that do not necessarily require the presence of an intellectual disabilities diagnosis. These states include both functional criteria that must be met (similar to those enumerated in the federal definition of developmental disabilities), and/or categorical definitions that specify particular conditions or diagnoses. Arizona, for example, requires a diagnosis of epilepsy, autism, cerebral palsy, or cognitive (intellectual) disability that occurred prior to age 18 years, and the presence of substantial functional limitations in three of seven major life areas.
An analysis of eligibility standards for HCBS programs in this study provided both consistent themes and variability across states. All states established that in order to be eligible to receive services under the HCBS waiver program, the individual would otherwise need long-term care in a nursing home or other institutional setting. Language such as “meeting an intermediate care facility (ICF-MR) level of care” was consistent across states. Income limits were also included in all state HCBS eligibility policy. For example, the majority of state policies indicated that the individual’s gross income must be below 300% of current maximum Supplemental Security Income benefit.
Individuals with autism also having a diagnosis of intellectual disability qualified for HCBS in each state. In terms of specific disability eligibility criteria, the majority of states used cognitive ability scores (i.e., IQ), functional limitation scores, or a combination of both to qualify for HCBS waiver services. Broad eligibility criteria such as diagnosis from a qualified professional (e.g., psychologist, physician, psychiatrist) or “meets DSM-IV criteria for disability” was also common in the eligibility language. The comprehensive HCBS waiver in many states included language about related conditions. An example of common state policy language about eligibility is as follows:
- The individual has a severe, chronic disability attributable to mental retardation, cerebral palsy, epilepsy, head injury, brain disease, ASD, or another condition that is closely related to mental retardation and requires treatment or services similar to those required for the mentally retarded. To be closely related to mental retardation, a condition must cause impairment of general intellectual functioning or adaptive behavior similar to that of mental retardation.
- The disability manifested itself before the individual reached the age of 22.
- The disability is likely to continue indefinitely.
Functional skill deficits were another common component of eligibility across states. The majority of states listed deficits in functional/adaptive skills (language/communication, learning, mobility, self-direction, capacity for independent living) as an aspect of eligibility. The standard across states was three or more functional needs to meet state eligibility criteria. Typical language was: “The individual must demonstrate significant or substantial functional limitations in three or more of the following major life activities: self-care, receptive and expressive language development and use, learning, self-direction, mobility, and capacity for independent living, with all occurring prior to the age of 18 years” (CMS, 2010).
Intelligence quotient (IQ) was a more complicated construct as it related to state eligibility criteria. For the majority of states that explicitly included IQ level as a component of eligibility criteria, the stated allowable IQ score had to be a standard score of 70 or below. A few states offered tiered IQ eligibility criteria with a different IQ cutoff point for related disabilities such as autism. For example, a few states, such as Florida, have one IQ requirement for people with intellectual disabilities (59 or less) and another threshold (69 or below) for people with secondary conditions such as autism. Some states, such as Georgia, indicated that persons with listed conditions other than intellectual disabilities qualify if they need similar types of services as persons with intellectual disabilities. Most states included more general terminology related to eligibility criteria, such as “[has a] diagnosis from a qualified professional” or “meets DSM-IVR criteria for MR or autism.” A few states used internal assessments or eligibility screeners for inclusion in the HCBS waiver.
Autism-Specific Waivers
An analysis of autism-specific waivers revealed that specific eligibility requirements were: (a) the diagnosis of an ASD by a qualified professional (licensed psychologist or physician) and (b) Medicaid income eligibility requirements. In these programs, IQ was not specified as a component of eligibility criteria (although for 1915(c) waivers, they also had to meet institutional level-of-care criteria). For children’s autism waivers, some states included financial eligibility statements, such as parents’ income (e.g., Colorado), while other states excluded parental income (e.g., Indiana, Maryland, Wisconsin). All children’s waivers included eligibility for the diagnosis of autism or ASD, but some states explicitly stated in policy that they extended services to children with Asperger’s syndrome, Pervasive Developmental Disorder-Not Otherwise Specified, and/or developmental disability. Diagnosis by a qualified professional such as a psychologist or pediatrician was required. Some states (e.g., Missouri) listed approved diagnostic screening tools (such as Childhood Autism Rating Scale; Gilliam Autism Rating Scale; Modified Checklist for Autism in Toddlers; Pervasive Developmental Disorders Screening Test, Second Edition; Autism Diagnostic Observation Scale Interview; Autism Diagnostic Interview, Revised; or Asperger Syndrome Diagnostic Scale). For the children’s autism waivers, some states specifically include children ages 8 years and younger (e.g., Colorado, Kansas, Massachusetts, Montana, South Carolina, Wisconsin), while other states extended eligibility from early childhood to young adulthood, such as ages birth-18, 3-18 or ages 1-21 (e.g., Maryland, Missouri, Nebraska, New York).
Eligibility for Adult Autism Waivers
For the waiver programs that provided supports to adults with autism, Indiana’s was designed to meet the needs of both children and adults. Pennsylvania’s specific adult autism waiver targeted adults age 21 and older. Maine has a combined program of HCBS for adults with intellectual disabilities or autism.
The Pennsylvania adult autism waiver limits eligibility to individuals with eligibility for Intermediate Care Facility for Persons with Other Related Conditions (ICF/ORC) or ICF-MR services. Individuals must have a diagnosis of ASD as determined by a qualified professional (e.g., licensed psychologist or physician) with the condition the disability manifested before the age of 22. Individuals also must display significant functional limitations in three or more major life activities as a result of the ASD. The Indiana autism waiver includes both adults and children with a diagnosis of ASD when qualifying as a developmental disability.
Services on Autism-Specific Waivers
Analysis of services provided in the children’s autism waivers reveals a focus on specialized needs of children with ASD, including intensive, in-home behavioral therapy (e.g., Applied Behavior Analysis), speech therapy, occupational therapy, social skills training, and children’s respite care. When comparing adult autism waivers to non-specific developmental disability waivers, there appeared to be some overlap in the services and supports provided. For example, common services listed under the specific adult autism waivers included adult day services, respite services, behavioral support, family training, environmental modification, and employment supports. Pennsylvania providers of support under the adult autism waiver are required to complete autism-specific training and meet specific standards related to autism. Clinical and behavioral support, as well as technical assistance, were also made available to enrolled providers under the waiver program. Additionally, the services provided had to be established as effective for people with autism and/or ASD.
Discussion
Autism spectrum disorders remain among the fastest growing developmental disability diagnosed in the U.S. (CDC, 2010), and many children currently identified with ASD will soon enter adult services at an increasing rate. The implication for major adult support systems is that the demand will significantly increase for services for individuals with ASD and their families. While tens of thousands of individuals with ASD are being served in state Medicaid HCBS waiver programs, there are serious challenges in meeting the needs of the growing number of individuals with ASD within the current programs, especially in states that do not have specific strategies to serve people with ASD in HCBS.
The purpose of this study was to collect data on how states serve individuals with ASD in Medicaid Home and Community Based Services. Specific questions included to what extent states served people with autism in HCBS programs, whether states provided a specific autism waiver, and if so, what eligibility criteria existed for autism services. A discussion of the policy trends observed in this study follows.
Autism, Intellectual Disability, and Functional Skills
In most states, the inclusion of people with autism and/or ASD in their primary HCBS program occurs because: (a) autism is explicitly included in the definition of eligibility as a related condition, (b) the person has a co-occuring intellectual disability, or (c) autism is included under the broader diagnostic umbrella of developmental disabilities. Historically, HCBS included people with ASD and their families and helped many individuals with ASD live in home and community settings and avoid institutionalization. However, since most HCBS programs limit services to individuals with intellectual disabilities and related conditions, in many states people with ASD must meet full criteria for an intellectual disability in order to qualify for HCBS waiver services.
In most states, the eligibility criteria for HCBS services include an IQ standard score below 70. Consequently, many individuals with ASD who do not have intellectual disabilities are not eligible for HCBS. While a significant percentage of people with ASD do have a co-occurring intellectual disability (American Psychiatric Association [DSM-IV-TR], 2000; Rutter, 2000), research suggests that a growing number of individuals receiving a current ASD diagnosis may not have a co-occurring intellectual disability (Edelson, 2006). Thus, a significant and growing percentage of people with ASD do not qualify for HCBS that require participants to meet institutional level of care criteria. In these situations, states need to explore additional HCBS options under the Medicaid program that do not require participants to meet institutional levels of care.
Functional skills were another primary component of state eligibility criteria under the state HCBS programs. It is well-documented in the research literature that many individuals with ASD but without intellectual disabilities still demonstrate significant needs in functional skills (Jacobson & Ackerman, 1990). Many of these individuals meet functional criteria guidelines based on developmental disability with significant functional limitations in three or more areas of major life activity. Many individuals with ASD who have borderline or average IQs have functional skills in areas such as communication skills, socialization, and community living that are considerably lower than would be predicted by IQ alone (Perry, Flannagan, Dunn Geier, & Freeman, 2009). For people with ASD, functional skills may be a better indicator of the skills needed to live independently and may be more directly related to the need for HCBS.
Autism Waivers for Children are a Growing Trend
A growing trend across states was the development of specific waivers for children with ASD. Several states had autism-specific waivers predominantly for children, and many indicated plans to develop a children’s autism waiver. The impetus to develop these waivers seemed to be in response to multiple factors, including growing demand, extensive waiting lists, and research confirming a critical window of intervention effectiveness during the early childhood years. Since most children with ASD do not receive a diagnosis until 3 years of age, access to service is needed quickly. The development of autism-specific children’s waivers helps to address this issue by providing more direct and expedient access to services for children with an autism diagnosis.
A review of children’s autism waivers across states revealed both similarities and differences in state policy. A common content denominator in state children’s waivers included a diagnosis of ASD and some states extended eligibility to other or broader disability categories such as Pervasive Developmental Disorders (PDD). Family support, Applied Behavior Analysis, and intensive behavioral interventions were commonly identified services and supports in these programs across states. However, there were relatively wide variations in the ages covered under the children’s waivers. Some states exclusively targeted the early childhood window (birth to age 5). Other states extended the age range from birth to age 21. Although specific age ranges for eligibility varied across states, all children’s autism waivers targeted children from birth to age 3. This policy is consistent with the growing body of research indicating that early childhood (birth to age 5) is a critical period for the effectiveness of behavioral, language, and other related therapies and interventions (Courchesne & Pierce, 2005; Dawson et al., 2009; Ozonoff & Cathcart, 1998). This policy focus on early intervention and effective supports might help the next generation of people with ASD fare better in the world of employment, community, and independent living.
Not only were the states with autism waivers for children part of a growing policy trend, states without autism-specific children’s waivers consistently indicated both the growing need and/or strong desire to develop specialized programs for children with autism. A few states indicated that they were in the preliminary planning stages of a children’s autism waiver, and many other states indicated that they hoped to develop a children’s program in the future. Current funding limitations were consistently cited as an obstacle to developing these waivers.
Autism Waivers for Adults are Less Common
A less common state policy trend was the development of adult autism waivers. At the time of data collection, two states had separate waivers that specifically served adults with autism. A closer look at the states that offer these programs reveals that eligibility criteria consists of a diagnosis of autism by a qualified professional. Intelligence quotient does not appear to be an eligibility requirement for the adult autism-specific waivers. There was some overlap with HCBS MR/DD waivers in terms of income and needs eligibility. Generally, adult autism waivers offer similar services as the primary HCBS programs for persons with intellectual and developmental disabilities, but with some services that address needs specific to adults with ASD.
Adult autism waivers appear to be a policy step towards addressing the needs of adults with ASD by offering specialized services and supports to that population. Previous research confirms that the quality of life for adults with ASD is directly associated with the quality of their supports and services (Renty & Roeyers, 2006). Because autism spectrum disorders are complex, heterogeneous disabilities, service systems need to be more specialized and targeted to address the unique service and support needs of individuals with ASD. Historically, there has been a lack of specialized support systems within communities that address the specific needs of people with ASD across the lifespan. Current research suggests that outcomes for adults with ASD are generally poor even when compared to other groups of adults with disabilities, including those with intellectual disabilities (Billstedt, Gillberg, & Gillberg, 2005; Saldana et al., 2009). Individuals with ASD often receive more costly services because of the pervasive, complex nature of their condition (Cimera & Cowan, 2009). The lack of service support coordination for adults with ASD may partly explain the poor outcomes and the expense of services. Autism-specific HCBS waivers have the potential to improve the service support match for individuals with ASD.
Rising Demand for ASD Services and Supports
As the prevalence of ASD diagnosis rises, demand for supports and services is expected to grow. States believe this growth will present significant policy challenges. State HCBS programs face lengthening waitlists and funding cuts. The 1915(c) waiver program functions as a “capped entitlement.” States limit the number of people enrolled in their waiver programs. While many states would like to increase the numbers of individuals served, declining state revenues and expanding Medicaid rolls have stifled growth. The mounting population of youth and young adults with ASD who are leaving school with substantial support needs increase the demands on an already-stressed adult service system. Those demands will increase in the coming years as the growing number of young people identified with ASD in early childhood progress through school and into the adult services system.
States in this study indicated a significant need for additional funding to meet the diverse needs of adults with ASD and their families. Funding limitations were consistently cited as a primary obstacle in the provision of specialized ASD services. Historically, ASD has been a very expensive disability to accommodate and states have been challenged to develop comprehensive, well-coordinated systems to support individuals with ASD. However, research suggests that the expense of lifelong supports can be reduced by as much as two-thirds with early diagnosis and appropriate intervention (Järbrink & Knapp, 2001). Furthermore, part of the challenge and expense may be that services are not always well-matched to the particular needs of the current population of individuals with ASD. In addition, it is possible that in the absence of specialized support systems, these individuals are likely appearing in other, more-costly support systems, such as mental health wards, emergency rooms, crisis placements or correctional facilities. Policy researchers may discover that less-costly community services addressing the long-term needs of people with higher functioning ASD could actually lower overall state costs.
States must also determine which services and supports are appropriately funded by private insurance and which are not. Capitation limits on lifetime expenditures and allowable private insurance expenditures have meant that private insurers have traditionally not funded long-term services and supports for people with lifelong disabilities. At the same time, many insurance companies do cover treatments and interventions, and an increasing number of ASD insurance bills are passing throughout the United States. It will be important for state policymakers to understand which needs are covered by private insurance, which are not, and then choose funding options for long-term care services that traditionally are not covered by private insurance.
Conclusion
Overall, the key findings of this policy review highlight the potential gap in services for individuals with ASD with significant functional limitations, but whose borderline or average IQ scores prevent them from receiving services. The proliferation of children’s autism waivers among states appears to be a policy development in response to growing need and research confirming the importance of early intervention. However, autism waivers for adults were not common across states.
The children who represent the first wave of what is commonly referred to as the “autism epidemic” are entering adulthood (Gerhardt, 2009). These adults will need an accessible system that provides services tailored to the needs of individuals with ASD. The current service delivery system faces significant challenges in the provision of quality lifespan services for individuals with ASD and their families, especially in adult ASD services. The current situation presents both an opportunity and a challenge to current service systems that are already overburdened and underfunded. There is an opportunity to structure the adult services system to address the specialized support needs of individuals with ASD and their families.
Much more information and research is needed to fully understand the effect and outcomes of ASD-specific Home and Community Based Services. A comparative analysis of outcomes of services for adults with ASD served through autism-only waivers versus general developmental disability waivers would provide a better understanding of what, if anything, is unique about ASD-specific HCBS and whether such services lead to superior outcomes for adults with ASD. Further investigation should also clarify whether there are differences in the characteristics (e.g., demographic, diagnostic, behavioral, and functional limitations and outcomes) of people with ASD, especially in autism-specific and general developmental disability waiver programs. In-depth interviews with policymakers in states with autism-specific waivers could identify how and why these waivers were developed and whether they meet expectations. More importantly, understanding the outcomes of state-specific programs will be essential in informing future ASD policy development.
States need to develop formal plans on how they will serve the increasing number of children with ASD diagnoses and their families across the lifespan. This influx of people with ASD will affect waitlists, expenses, and the long-term viability of state programs. States should consider using a functional limitation criteria for adults with ASD so individuals with significant support needs, but no intellectual limitations, can still get their needs met. States must also ensure that service providers, practitioners, and direct support workers are prepared to meet the specific needs of children and adults with ASD.
References
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (Revised 4th ed.). Washington, DC: Author.
Baird, G, Simonoff, E, Pickles, A., Chandler, S., Loucas, T., Meldrum, D., & Charman, T. (2006). Prevalence of disorders of the autism spectrum in a population cohort of children in South Thames: The Special Needs and Autism Project (SNAP). Lancet, 368(9531), 210-215.
Billstedt, E., Gillberg, I. C., & Gillberg, C. (2005). Autism after adolescence: Population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders, 35, 351-360.
Brugha, T., McManus, S., Meltzer, H., Smith, J., Scott, F. J., Purdon, S., Harris, J., & Bankart, J. (2009). Autism Spectrum Disorders in adults living in households throughout England – Report from the Adult Psychiatric Morbidity Survey 2007. London: The NHS Information Centre for Health & Social Care.
Cavagnaro, A. T. (2007). Autistic Spectrum Disorders: Changes in the California caseload, An update: June 1987-June 2007. Sacramento, CA: California Health and Human Services Agency.
Centers for Disease Control and Prevention (CDC). (2010). Autism spectrum disorders: Data and statistics. Retrieved December 2010 from http://www.cdc.gov/ncbdd/ASD/data.html
Centers for Medicare and Medicaid Services (CMS). (2010). Medicaid waivers and demonstration list. Retrieved March 2010 from https://www.cms.gov/medicaidstwaivprogdemopgi/mwdl/list.asp
Cimera, R. E., & Cowan, R. J. (2009). The costs of services and employment outcomes achieved by adults with autism in the U.S. Autism, 13(3), 285-302.
Courchesne, E., & Pierce, K. (2005). Why the frontal cortex in autism might be talking only to itself: Local over-connectivity but long-distance disconnection. Current Opinion in Neurobiology, 15(2), 225-230.
Dawson, G., Rogers, S., Munson, J., Smith, M., Winter, J., Greenson, J., Donaldson, A., & Varley, J. (2009). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125(1), 17-23.
Edelson, M. G. (2006). Are the majority of children with autism mentally retarded? A systematic evaluation of the data. Focus on Autism and Other Developmental Disabilities, 21, 66-83.
Eaves, L. C., & Ho, H. H. (2008). Young adult outcomes of autism spectrum disorders. Journal of Autism and Developmental Disorders, 38(4), 739-747.
Freedman, R. I., & Boyer, N. C. (2000). The power to choose: Supports for families caring for individuals with developmental disabilities. Health and Social Work, 25, 59-68.
Ganz, M. (2006). The costs of autism. In S. O. Moldin & J. L. R. Rubenstein (Eds.), Understanding Autism (pp. 475-502). Boca Raton, FL: Taylor & Francis.
Ganz, M. (2007). The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics and Adolescent Medicine, 161, 343-349.
Gerhardt, P. (2009). The current state of services for adults with autism. Advancing Futures for Adults with Autism: Think Tank. Arlington, VA: Organization for Autism Research.
Howlin, P., Goode, S., Hutton, J., & Rutter, M. (2004). Adult outcome for children with autism. Journal of Child Psychology & Psychiatry, 45(2), 212-229.
Hurlbutt, K. & Chalmers, L. (2004). Employment and adults with Asperger syndrome. Focus on Autism and Other Developmental Disabilities, 19(4), 215-222.
Hurth, J., Shaw, E., Izeman, S. G., Whaley, K., & Rogers, S. J. (1999). Areas of agreement about effective practices among programs serving young children with autism spectrum disorder. Infants and Young Children, 12(2), 17-26.
Jacobson, J. W., & Ackerman, L. J. (1990). Differences in adaptive functioning among people with autism or mental retardation. Journal of Autism and Developmental Disorders, 20, 205-219.
Jacobson, J., Mulick, J., & Green, G. (1998). Cost-benefit estimates for early intensive behavioral intervention for young children with autism: General model and single state case. Behavioral Interventions, 13, 201-226.
Järbrink, K., & Knapp, M. (2001). The economic impact of autism in Britain. Autism, 5, 1, 7-22.
Johnson, D., & Myers, S. (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics, 120(5), 1183-1215.
Kim, Y. S., Leventhal, B. L., Koh, Y. J., Fombonne, E., Laska, E., Lim, E. C., Cheon, K. A., Kim, S. J., Kim, Y. K., Lee, H. K., Song, D. H., & Grinker, R. R. (2011). Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry, 168(9), 904-912.
Kogan, M., Blumberg, S., Schieve, L., Boyle, C., Perrin, J., Ghandour, R., Singh, G., Strickland, B., Trevathan, E., & van Dyck, P. (2009). Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the U.S., 2007. Pediatrics, 124(5), 1395-1403.
Lakin, K. C., Larson, S., Salmi, P., & Webster, A. (Eds.). (2010). Residential services for persons with developmental disabilities: Status and trends through 2009. Minneapolis, MN: University of Minnesota, Institute on Community Integration, Research and Training Center on Community Living.
Larson, S. A., & Lakin, K. C. (2010). Changes in the primary diagnosis of students with intellectual or developmental disabilities ages 6 to 21 receiving special education services, 1999 to 2008. Intellectual and Developmental Disabilities, 48(3), 233-238.
Lord, C., & Bishop, S. (2009). The autism spectrum: Definitions, assessment and diagnoses. British Journal of Hospital Medicine, 70(3), 132-135.
Mawhood, L., Howlin, P., & Rutter, M. (2000). Autism and developmental receptive language disorder – A comparative follow-up in early adult life: Cognitive and language outcomes. Journal of Child Psychology and Psychiatry, 41(5), 547-559.
National Core Indicators. (2008). What does NCI tell us about people with autism? National Core Indicators Data Brief, 6(2), 1-7.
Ozonoff, S., & Cathcart, K. (1998). Effectiveness of a home program intervention for young children with autism. Journal of Autism and Developmental Disorders, 28(1), 25-32.
Perry, A., Flanagan, H. E., Dunn Geier, J., & Freeman, N. L. (2009). Brief report: Vineland Adaptive Behavior Scales in young children with autism spectrum disorders at different cognitive levels. Journal of Autism and Developmental Disorders, 39(7), 1066-1078.
Renty, J., & Roeyers, H. (2006). Quality of life in high-functioning adults with autism spectrum disorder: The predictive value of disability and support characteristics. Autism, 10(5), 511-524.
Rutter, M. (2000). Genetic studies of autism: From the 1970s into the millenium. Journal of Abnormal Child Psychology, 28, 3-14.
Saldana, D., Alvarez, R. M., Lobaton, S., Lopez, A. M., Moreno, M., & Rojano, M. (2009). Objective and subjective quality of life in adults with autism spectrum disorders in southern Spain. Autism, 13(3), 303-316.
Uddin, L. Q., Menom, V., Young, C. B., Ryal, S., Chen, T., Khouzam, A., Minshew, N. J., & Harden, A. Y. (2011). Multivariate searchlight classification of structural magnetic resonance imaging in children and adolescents with autism. Biological Psychiatry, 70, 833-841.
U.S. Government Accountability Office. (2006). Federal autism activities: Funding for research has increased, but agencies need to resolve surveillance challenges (GAO Publication No. GAO-06-700). Washington, DC: Author.
U.S. State Education Data, Office of Special Education Programs. (2003). Twenty-fifth annual report to Congress on the implementation of the Individuals With Disabilities Education Act. Washington, DC: U.S. Department of Education, Office of Special Education Programs.
Zaharia, R., & Moseley, C. R. (2008). State strategies for determining eligibility and level of care for ICF-MR and waiver program participants. New Brunswick, NJ: Rutgers Center for State Health Policy.
This publication is supported, in part, by Cooperative Agreement #H133B080005 from the National Institute on Disability and Rehabilitation Research (NIDRR), U.S. Department of Education.
The opinions expressed in Policy Research Brief are those of the authors and do not necessarily reflect the position of the Center or its funding sources.
Print copies of this publication are available for $3.00 per copy. An order form is available online, or contact:
Publications Office
Institute on Community Integration
University of Minnesota
109 Pattee Hall
150 Pillsbury Drive SE
Minneapolis, MN 55455
612/624-4512
icipub@umn.edu
Policy Research Brief is available in alternative formats upon request from the above address.
The University of Minnesota is an equal opportunity employer and educator.
Published on the Web site of the Institute on Community Integration, University of Minnesota (http://ici.umn.edu)